The healthcare industry has reached an inflection point where affordable healthcare and traditional healthcare interventions that begin in the hospitals are not adequate. The industry is grappling with issues such as an increase in the number of chronically ill, and the aging population and their myriad of health related challenges.
The need of the hour is to change the approach to healthcare; health consumers and the overall community must take proactive measures to prevent chronic illness, which will improve patient outcomes and reduce total costs. Healthcare delivery needs to move closer to the patients, to right where they live. This approach requires identifying Social Determinants of Health (SDoH), the conditions in which people live and the larger forces that shape their daily life. Identification and integration of SDoH with clinical data can help healthcare providers generate insights and deliver suitable interventions effectively.
“If we want to make our patients well, that means we want to make our communities well. Moreover, that means prevention and addressing the social determinants of illness”
Social Determinants of Health (SDoH)
The World Health Organization defines SDoH as the conditions in which people are born, grow, work, live, and age and the wider set of forces and systems shaping the conditions of daily life.
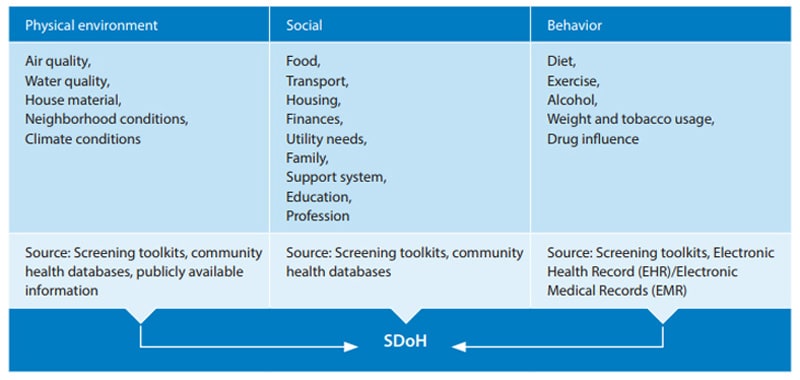
Population health is focused on understanding the full range of fundamental upstream causes of health issues, and managing valuable or risky determinants in a specific population to prevent the onset of a medical condition.
SDoH can be effectively used to manage population health in multiple ways, like:
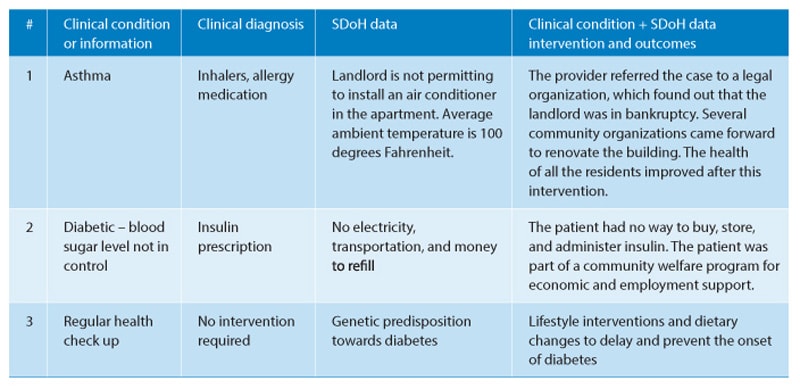
1. To identify and recognize SDoH and provide interventions based on the collected data. Table 1 lists certain use cases that highlight the importance of SDoH in determining the root cause
Table 1: SDoH, root cause, and intervention
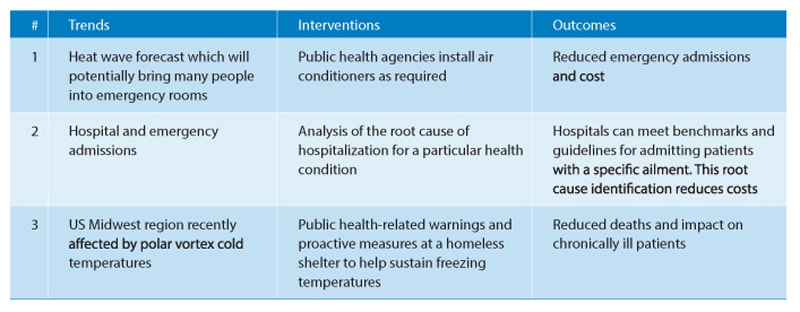
2. To uncover patterns connecting health determinants with community-level trends at a population or hospital level. Table 2 lists certain use cases illustrating the use of trends and patterns to provide interventions.
Table 2: Community level trends, interventions, and outcomes
To discover at-risk population and predict complications before they occur.
To risk-stratify patients (high, moderate or low) based on SDoH as well as clinical data and chart how certain health determinant factors can influence treatment and disease outcomes. With timely interventions, this process can reduce the risk of a patient moving to a chronic disease state. As a majority of these interventions are not clinical, healthcare providers will play the primary role to connect patients with community related care providers and other welfare providers.
The integrated process of population health
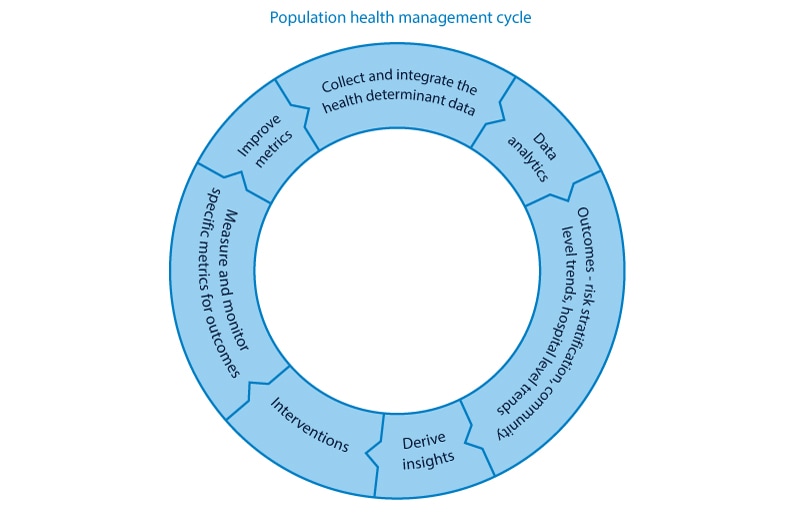
The possibilities of identifying meaningful insights and use cases based on SDoH and potential benefits that arise out of it are essentially limitless, provided the health ecosystem stakeholders pursue the integrated process of population health.
The logical steps in the integrated process of population health are:
- Collect all related meaningful data from the health determinants.
- Integrate data from all determinants with clinical information.
- Apply advanced analytics to combine, analyze, visualize, and derive useful insights.
- Provide appropriate interventions based on the insights to drive better patient outcomes.
- This process is a cyclical process; we need to continuously work on all the steps and improve metrics with each cycle.
Factors that influence the adoption of population health based on SDoH
Payors seek increased participation in value-based reimbursement models which focus on outcomes.
Hospitals in provider networks have financial incentives to meet certain quality benchmarks, focus on prevention, and manage population health. They get paid to keep patients out of the hospital.
Healthcare system understanding that fixing upstream issues and root causes will reduce costs and that prescription is not a solution to every healthcare problem.
Challenges to SDoH adoption

50% healthcare and life sciences firms have said that the integration of multiple data sets from various sources was the biggest challenge in implementing analytics-led initiatives.
- Data integration and interoperability
- Behavioral changes
- Network registries
- Data privacy
Healthcare system users leave a trail of data in every interaction with the system – be it with the provider, payer, diagnostic center, and other sources. Integrating and accessing information from fragmented data origination systems (characterized by varying data quality) and file formats is complicated and is a significant industry challenge.
Changing the behavior of physicians by encouraging them to provide interventions like connecting patients with welfare programs.
Providers currently don’t have access to a good network of community welfare providers for patient referrals.
There will be data privacy concerns for patients since it involves sharing their personal information.
Technology opportunities and solutions
- Educate providers on the importance and significance of SDoH through the current platforms they use. Electronic Health Record (EHR) providers can use their platforms to promote awareness.
- Use social media networks like Facebook and Twitter to promote awareness and importance of sharing SDoH data at the point of care.
- Mask data for personal identity when shared for aggregate level trend analysis.
- Develop screening toolkits to collect social determinant data, with patient psychology in mind. Several research studies are underway in this area. Design digital solutions into screening toolkits, around the patient, with an intuitive design that requires minimal input. Infosys has developed a Blockchain platform to allow every entity in the healthcare value stream to work together in an interoperable transparent model to ease the collection of SDoH data.
- SDoH digital solutions in the space should focus on data interoperability based on potential integrators and the different standards evolving in the health exchange market. Standards like SMART on FHIR and CDA are becoming popular as they facilitate data exchange and interoperability. These standards also present results in a simple, intuitive, and comprehensive way.
- SDoH issues require cooperation between patients, providers, community groups, and local health providers. Cloud-based solutions can address data sharing, but data flow must be seamless.
- Predictive analytics solutions are emerging. Many healthcare providers use off-the-shelf products, which can augment their existing EHR systems and support the analytics function. Infosys researched this area and is using the results to develop screening tools powered by artificial intelligence (AI) and automation.
- There are several emerging community network registries. These databases provide information on human support services, which can be accessed by providers and caregivers for non-clinical interventions. NowPow and Aunt Bertha provide referral solutions and connect providers with social services.
- Referral platforms can operate with other platforms to improve data transfer.
- Payer companies can leverage publicly available data like census reports and combine it with their claims data. Further, payers can use AI to develop predictive modeling and holistic risk stratification models.
A healthier future
SDoH is already a well-respected field of study. However, technology support for SDoH is still emerging and is an exciting area with significant potential. The global health community is aware of the importance of SDoH to address the rise of chronic diseases worldwide. EHR vendors have also shown keen interest to include SDoH information on their platforms.
To realize the full potential of SDoH, providers need to upgrade their IT infrastructure and improve workflow integration, analytics, and community resource referral. All stakeholders in the healthcare system have greater incentive to invest in population health technologies with a shift toward value-based care. SDoH is an incredible opportunity to improve our population health through a combination of technology solutions and humanistic interventions