The spread of COVID-19 has broken the weak links in the health care supply chain, with the greatest impacts falling on health care professionals and their patients. What were chronic problems before the pandemic, have progressed into a series of acute supply chain failures that have limited and delayed COVID-19 testing1 and contributed to shortages of critical medical equipment.2
In the pre-COVID-19 era, health care providers and their suppliers built lean and efficient supply chains. But those systems come with walls and silos, and do not connect to the patient and to medical outcomes.
In pursuit of efficiency, health care has joined most industries in pursuing just-in-time supply models and group purchasing, both of which are sensible from a cost-control perspective. But just-in-time supply systems don’t allow for rapid scaling for increased activity or sudden shocks to the availability of supplies and raw materials. Further, consolidation and pooled buying practices of group purchasing organizations layer in complexity and reduce agility. Critics of GPOs also argue that these arrangements and their fee structures discourage competition and innovation.3
In 2017, Hurricane Maria struck Puerto Rico and foreshadowed the disruption that the new coronavirus is now delivering. Pharmaceutical providers and medical supply companies had consolidated production of certain medicines and supplies in Puerto Rico. In addition to the human devastation suffered by Puerto Ricans, the health care supply chain in the U.S. faced shortages of IV solution bags, antibiotics and insulin pumps.4
The push for efficiency in the health care supply chain has not led to better visibility or integration across ecosystems. Health care providers have not created a full view of the patient experience across the health care supply chain because of the legacy walls and silos in their ecosystems. For example, the wall between the supply chain and medical records makes linking products and outcomes impossible. Supply chain usage in the majority of health systems is not linked to electronic health records.5 Supply chain data does not connect to the reimbursement processes and payer contractual payment models.
A focus on patients and transparency
Placing patients at the center of a rebuilt supply chain will lead to a more resilient system. With patients and outcomes at the center, all stakeholders can share data more broadly. Further, a singular, patient-centered view will enable more responsiveness and better planning for suppliers, caregivers, institutions and communities. A unified, resilient and adaptable system is an essential tool to prepare for future pandemics and possible aftershock outbreaks of COVID-19.
Consider how triage would function differently in a fully visible, patient-centered context. Typically, a person with symptoms shows up at an emergency room and mingles with noninfected patients. A well-supplied and well-informed system could reach the potential patient before the patient reaches the hospital. Institutions and governments could deploy in-field screening facilities based on data, predictive analytics and clinical algorithms. Such a triage system could guide patients to the most appropriate site for care, which would reduce the strain on emergency rooms and align caregivers with their suppliers in efficient ways.
The pandemic has proved that the absence of a full, patient-centered view impacts all health care aspects right from disaster planning to work force management
To be sure, health care systems and health care technology businesses have been pursuing the goal of getting a full view of the patient, but mostly in a clinical context. The pandemic highlights that this lack of a full, patient-centered view impacts all aspects of health care — disaster planning, work force management, provider practices and delivery of primary care. If executives in the supply chain could see all the way to the patient, they could more quickly see stresses on the supply chain and adapt. A singular, transparent, patient-centered view now must be a goal for the entire health care ecosystem. A more transparent supply chain with full connections to clinical data will reveal weak points before they are stressed in times of crisis. But that will require all stakeholders to share data in greater detail, which could reveal sensitive topics from the provider and vendor side. A broader supply chain must remove walls and silos that currently exist and include a wider universe of parties and data sources, such as real-world evidence and real-world data.6
Tying improved outcomes to reimbursement and showing true costs can incentivize health care stakeholders to commit to broader data sharing and integration. Implementing and integrating digital systems can assist in simplifying that effort.
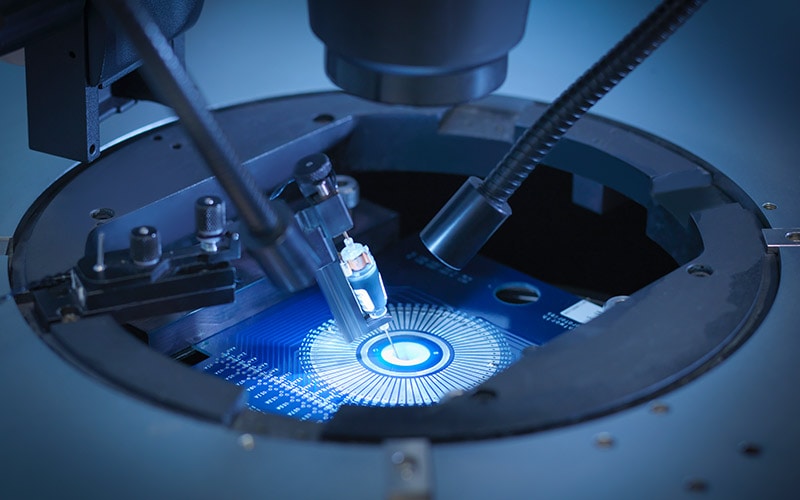
Figure 1. A supply chain of the future provides more transparency and a wider view of the entire system.

A system slow to integrate
Relative to other industries, health care has been slow to integrate all its data. According to the Infosys Knowledge Institute’s Digital Radar 2020 survey of digital maturity, 30% of health care organizations surveyed had fully upgraded legacy systems.7 Fully connecting health care data remains a big challenge. Health care providers and institutions often cobble together a mix of disconnected IT systems to deliver care. It remains extremely difficult to build insight into how providers use supplies across sites and procedures. Some providers and distributors were working to improve upon this while making efforts to standardize the contracting process. Still, distributors and health systems do not share data, leaving them unable to jointly assess waste in the supply chain. Even in the midst of a pandemic, institutions remain reluctant to share supply inventory.8
Enterprise resource planning software that is a mainstay in other industries has not really arrived in health care, because ERPs have historically been too big or expensive for hospital systems. But that has begun to change.9 Full connection is growing more appealing and possible. Health care providers are seeing profit pressure from new, unconventional competitors such as CVS Health and Amazon, which has prompted systems to seek a fuller view of their spending. Care providers who implement ERP platforms to better grasp their costs have the opportunity to link those to digital medical records and create a fully connected view of cost, patient care and the supply chain.10
Figure 2. Digital advances make costs more visible.10

COVID-19 reinforces the need for hospital systems to have better planning tools and insight into health care, starting with a fully connected digital supply chain. Take the example of New Orleans-based Ochsner Health. The head of the regional health system describes staffing issues as its greatest challenge in the first month of pandemic response.11 Hospitals have typically sourced workforce management to their human resources department or to a third-party vendor, which results in immense and costly variations in terms of access to care, patient care quality, and patient and workforce safety. The addition of a resource planning framework that can be integrated with a fully digital and connected supply chain will provide visibility to resource needs in terms of people and supplies.
Steps toward a resilient, robust and adaptable supply chain
To build a fully connected supply chain requires the willingness of a range of stakeholders, each with divergent motivations, to find common ground and common motivations. Higher quality, broader availability of care and improved customer service can serve as uniting factors. Once the stakeholders are united and oriented in the same direction, they can collaborate and find ways to:
- Place the patient at the center of the health care supply chain.
- Integrate patient and system data as broadly as possible.
- Link outcomes to reimbursement across the health care supply chain.
- Provide visibility for all parties.
- Find ways to harmonize just-in-time manufacturing with disaster preparedness.
- Calculate the true costs of each stage of the supply chain.
The COVID-19 pandemic has highlighted the complexity and weaknesses of the global health care supply chain. It has also reinforced the need for greater transparency across the health care ecosystem. Whether as a result of government mandates, public pressure or lessons learned, suppliers, caregivers and other stakeholders have added incentives to do better. These groups can put digital systems to work in building a more resilient health care supply chain centered on the patient.
References
- Hospital Experiences Responding to the COVID-19 Pandemic: Results of a National Pulse Survey, Christi A. Grimm, April 2020, U.S. Department of Health and Human Services Office of the Inspector General.
- “Doctors Say Shortage of Protective Gear Is Dire,” Andrew Jacobs, Matt Richtel and Mike Baker, March 19, 2020, The New York Times.
- The Role of Group Purchasing Organizations (GPOs) in the U.S. Medical Industry Supply Chain, Bernard Weinstein, 2006, Estudios de Economia Aplicada.
- “Hurricane Maria Takes a Toll on Global Medical Supplies,” Adam Aton, Oct. 25, 2017, Scientific American.
- EHR supply chain fusion, Karen Conway, Nov. 18, 2014, Policy and Value-Based Care.
- Real world data: An opportunity to supplement existing evidence for the use of long-established medicines in health care decision making, Vaibhav B. Katkade, Kafi N. Sanders and Kelly H. Zou, July 2, 2018, Journal of Multidisciplinary Healthcare.
- Infosys Digital Radar 2020: Breaking through the Digital Ceiling, Jeff Kavanaugh and Chad Watt, Jan. 26, 2020, Infosys Knowledge Institute.
- Coronavirus Pushes More Hospitals To Share Data About Inventories Of Protective Gear, Blake Farmer, March 12, 2020, National Public Radio.
- ERP Software in Healthcare: How is it Helping?, Sarah Morris, April 1, 2019, Healthcare Technology.
- What happens to health care as more of the cost burden shifts to the patient?, Mark Weber, Dec. 6, 2018, Becker’s Hospital Review.
- Anatomy of Ochsner Health’s COVID-19 Response, Mandy Roth, April 3, 2020, Health Leaders.